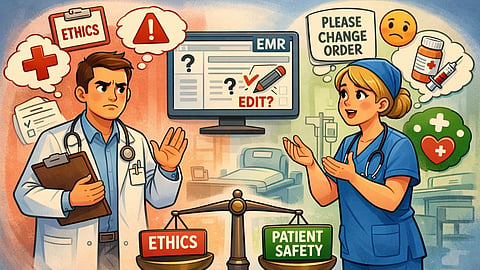
In an anonymous online discussion among U.S.-based physicians, a troubling incident in the emergency department (ED) sparked a debate over medical ethics, medication error documentation, and professional responsibility. The conversation highlighted the difficult decisions doctors face when medication errors occur and the pressures they sometimes experience from staff, particularly nurses, to alter existing records to prevent such incidents from being reported to authorities.
A physician shared his troublesome experience with a nurse:
“Last night, while working in the ED, I ordered 30 mg of Toradol IV. I was approached by a new nurse and her preceptor, who told me she had pulled the wrong concentration of the drug and gave 60 mg IV.”
He further added, “They asked me to change my order to match what she had given. I refused, saying that was not the dose I ordered and that they have a way to document medication administration errors, which is what they should do. I would not take responsibility for the wrong dosage being given.”
The doctor then admitted that he felt tempted to adjust the record and wrote, “I was tempted to change the order and then write a note stating that I had ordered a different dosage, but I was asked by the nursing staff to change the record. I felt that would have been passive-aggressive and worse.”
This incident was not isolated. The physician highlighted a similar situation involving a colleague:
“A similar thing happened to another doctor I work with when she ordered a dose of Decadron. That dose was given, but another nurse thought she heard Solu-Medrol and gave that as well. A week later, the assistant director asked her to go into the computer system and place an additional order for the Solu-Medrol (which she actually never ordered) because it would appease the nurses. She refused to do that as well.”
The post raised a central ethical question: