OBG/Gynae Physiotherapy Explained – Dr. Juhi Saxena on Pregnancy, Delivery, Pelvic Floor Health, Post-natal Care (Part-4)
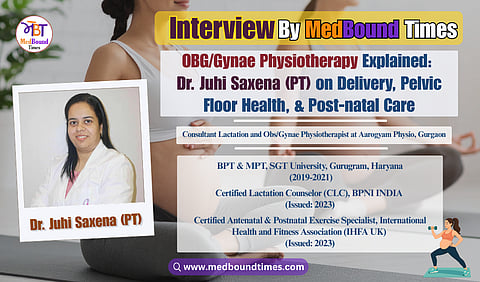
Many people still aren’t aware that OBG/Gynae physiotherapy exists—or how much it can improve women’s health at different stages of life. To spread awareness about this important and lesser-known aspect of physiotherapy, Dr. Pooja Bansal (PT) and Himani Negi from Medbound Times spoke with Dr. Juhi Saxena (PT), a women’s health physiotherapist.
Currently serving as a Consultant Lactation and Obs/Gynae Physiotherapist at Aarogyam Physio, Gurgaon, she has been actively working to raise awareness about this specialized field.
With a Bachelor’s degree in Physiotherapy from SGT University and a Master’s in Obs and Gynae Physiotherapy from the same institution, she highlights in this interview how physiotherapy plays a vital role in managing pregnancy-related discomfort, supporting postnatal recovery, addressing pelvic floor issues, and promoting overall wellness.
Himani Negi: We were discussing normal delivery and C-section, a topic that is still considered taboo. In our conversation with Dr. Soujanya Banka from South India, she explained that while C-sections might seem easier, it is actually very painful, with slower healing, and are often reserved for emergencies. The goal is usually a normal delivery, and even the government has set norms for C-sections.
However, many people—including my mom—believe that private hospitals push for C-sections, so they prefer government hospitals. If a woman strongly wants a normal delivery, can she prepare for it in advance? Can a physiotherapist help assess and guide her beforehand, even if she has concerns like a narrow pelvic floor? At what stage should she start, and can this be done even in smaller towns with limited physiotherapy access?
Dr. Juhi Saxena (PT): That’s the difference. If you’re a gynae physio, you don’t prepare a mother only for a normal delivery—you prepare her for the delivery. Ninety-nine percent of things may be in our control, but there’s always that 1% that can change unexpectedly. Our goal is a healthy birth and bonding—a happy, healthy mother and baby.
Our focus is 90% towards normal vaginal delivery, but there’s a myth here. Normal delivery means minimal or no assistance—no episiotomy, no perineal tear. If there’s a cut or tear, it’s a vaginal delivery, but not a normal one. Unfortunately, people often label any vaginal birth as “normal,” even when it involves cuts or stitches. And whether it’s a vaginal tear or a C-section incision, you’re still getting a cut—both have challenges.
What’s most important is preparing the mother to make informed decisions:
“If I face certain complications, I can confidently opt for a C-section,” or “I can safely continue with a vaginal birth.”
No one tells mothers in advance about the possible post-delivery issues from perineal tears or episiotomy—urinary problems, constipation, and difficulty sitting. Later, some mothers even say, “I wish I had gone for a C-section.”
From my experience, a C-section is also not easy. After surgery, many mothers spend 24–48 hours in severe discomfort. For the first 6–8 hours, they may not even be allowed water. Lying still for 24 hours is traumatizing, and the first attempt to move can feel overwhelming. Both methods have pros and cons—it’s about understanding and accepting them.
If someone wants to prepare for a vaginal delivery, yes, consulting a physiotherapist can help. If you reach us by the second trimester, we can do a thorough assessment. Even in remote areas, online sessions work well. At least 70% of the assessment can be done through online mode, and some parts may require in-person visits. During COVID, I guided several first-time mothers remotely, and most had successful vaginal deliveries. The key is finding the right professional and staying connected.
Dr. Pooja Bansal (PT): We know pregnancy takes a toll emotionally, physically, and mentally. How important is physiotherapy or exercise in helping women cope better?
Dr. Juhi Saxena (PT): Exercise benefits are widely documented, but what we often overlook is the feel-good factor. Under proper guidance, exercise builds motivation and accountability—you stick to it because someone is guiding and checking in. Without that structure, it’s easy to stop. Light exercises, done consistently, keep you active, improve mood, and once you start feeling the results, you naturally want to continue—that’s when the real benefits appear.
Dr. Pooja Bansal (PT): The postpartum phase can be just as challenging as pregnancy. Many women face postpartum depression or neglect their own health while caring for the baby—and unfortunately, this is often even celebrated. People say, “Now that delivery is done, just focus on the baby.” How do you counsel such patients or their families so they also focus on the mother’s health?
Dr. Juhi Saxena (PT): Yes, we have been talking about pregnancy in this interview as well, and we’ve discussed it a lot. Now, I will shift to the postpartum phase. We often use the term jacha-bacha—it is a Hindi phrase. If we want the baby (bacha) to be healthy/good, then the jacha (mother) must also be strong. So to have a healthy and happy baby, you first need to have a healthy and happy mother.
So here comes the trick of wordplay. It’s about how well you’re playing with your words, with the attendants, with the family. If you see that the baby is their weak point, catch hold of that baby—revolve the conversation around the baby and connect the mother to the baby emotionally. For some households, it’s the household work that matters the most—catch hold of that aspect, and connect your guidance to their specific demands.
When you modulate your words around it, that’s when you’ll get a good response from the family. If you keep forcing things, they won’t understand—because it’s not connected to them. You need to connect with them on a level they understand.
Dr. Pooja Bansal (PT): Alright, coming to post-pregnancy, many women face pelvic floor issues. How can physical therapy help them manage or reverse these problems? What role do we play?
Dr. Juhi Saxena (PT): Pelvic floor issues can be seen in girls as young as 10 or 12, and also in women in their seventies with prolapse, urinary leakage, and so on.
I have seen cases where a woman has never delivered or been pregnant, yet she still faces pelvic floor issues. So tagging it only with childbearing is not a good or ideal approach.
The pelvic floor is just like any other muscle in your body. But while all our other muscles are generally looked after, the pelvic floor is the most neglected one. If we’ve already neglected it, then getting it back to baseline and developing it is a task. Whereas with other muscles, we’re usually aware and trained, so with the pelvic floor being underrated, it becomes a double challenge to train it.
If, during pregnancy, we teach the mother the right way to do things—how to carry herself and how to take care of her pelvic floor—there are very few chances she will come back to us in the postpartum phase with pelvic floor issues. But if there has been no guidance, and the birthing was traumatizing or something incidental, then the mother is more likely to return with these issues.
When someone comes to us with a pelvic floor problem, we shouldn’t keep blaming it on their history, the thing we do the most often. Remember, you can’t change the past, but you can only build from what's in the present. If she has a weak pelvic floor, then explain to her or the attendant the possible reasons, but stop nagging about it and start working from here.
For example, if she had a traumatizing birth and comes to me four months later with urine leakage, I’ll explain that it happened because of that. She should be aware of it, but then we stop talking about what’s already happened and focus on building from now on.
Setting small, achievable goals will keep the mother motivated and help us track her progress toward the bigger targets. If on day one we target only “controlling urine,” that’s a long-term goal. For now, we can focus on reducing the number of her washroom visits—that’s also an achievement.
We should celebrate these small wins because they keep the mother motivated and help her stay committed to the program until she reaches her goals.