Around the same time, Wen Yih Aw, PhD, was working as a postdoctoral researcher at UNC Catalyst, a research group focused on understanding rare diseases in the Eshelman School of Pharmacy. Aw was collaborating with the Polacheck lab on a vascular Ehlers Danlos Syndrome project. Eventually, Aw joined the Polacheck lab and used her molecular biology expertise to help develop the VMs model.
In addition to Dr. Blatt and Aw, the lab has an on-going collaboration with Boyce Griffith, PhD in the Department of Mathematics and the Computational Medicine Program at the UNC College of Arts and Sciences, who is helping with analyzing the structures of the networks.
“All those pieces were necessary to complete the work,” said Polacheck. “It does say something about UNC-Chapel Hill because there were multiple departments across campus involved. There were no barriers whatsoever to working together on this project.”
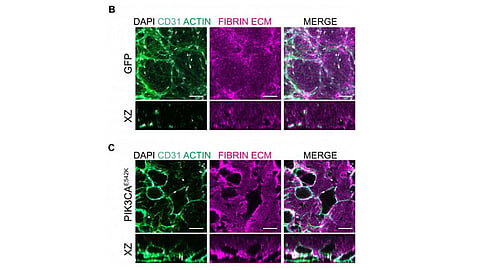
Microfluidic models are incredibly small – about the size of a millimeter – three-dimensional devices that can be used to control or simulate the environment within the body. In this case, a small piece of blood vessel composed of healthy human endothelial cells or endothelial cells expressing the PIK3CA mutation is centered inside of the device. From there, the researchers can look into the process of vascular formation, and introduce specific chemicals and mechanical forces to the model to simulate the conditions of the body. They observed formation of enlarged and irregular vasculature with the introduction of PIK3CA mutation.
To confirm whether or not their model accurately portrays the manifestation of the disease, the team next conducted a drug efficacy study.
There are two drugs currently used for the treatment of vascular malformations: rapamycin and alpelisib. The latter is a newly discovered PIK3CA-specific inhibitor recently approved by the FDA to treat certain types of breast cancer and PIK3CA-related overgrowth spectrum. So far, pre-clinical studies in mouse models and in patients have shown that alpelisib is more effective in reversing vascular malformation defects.
After selecting the two drugs, Polacheck and Aw applied the treatment to their devices. The study was a success.
“The blood vessels used to be really dilated and large,” said Aw, first author of the study. “By imaging the vessels before and after treating with drugs, we observed the vessels shrink and, more or less, revert it back to a normal shape and function. We were very excited to be able to replicate some of the results in vitro with the model we built.”
Moving forward, Aw and Polacheck are looking to replicate the finding in tissues from vascular malformation patients, especially those who don’t have the PIK3CA mutation or don’t have clear genetic information. Their model can now be used to evaluate new medications or to perform synergistic drug studies.
Now that they know that their model works, Aw and Polacheck plan to use it to study the behavior of the mutated cells overtime, as well as how the mutation affects malformations of the lymphatic tissue.
The disease initially begins with an individual cell that acquires the PIK3CA mutation. Then, much like a chain reaction, the effects of the mutation in that one cell spreads to the surrounding cells until the malformation is fully formed. As their model currently stands, the lab cannot mimic that natural process.
Aw is currently working on a new and different approach for a microfluidic model. She aims to create a platform that will allow them to start with cells that are healthy, and then “flip on” the mutation, and watch it progress across the tissue of interest. Ultimately, it will help them understand how the mutation is able to affect other cells and move throughout space.
Vascular malformations can also occur in lymphatic tissue. As opposed to blood vessels, lymphatic vessels have a duty to recycle excess fluid throughout the body and acts as a superhighway for immune cells to get to sites of infection. Very little is known about the basic cell biology of lymphatic endothelial cells, so Polacheck is hoping to do a study that is similar to his most recent one.
“The outputs are slightly different because the function of the lymphatics is different from blood vessels,” said Polacheck. “By comparing and contrasting what happens on the blood side and the lymphatic side, we will also be able to learn something about the basic biology of those two types of tissues.” (MSM/Newswise)
Hurry up! Join the Medical Internship 3.0 at MedBound!