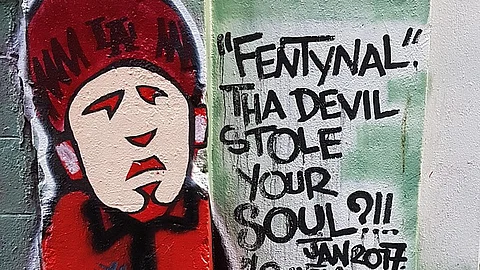
Despite what scientific evidence suggests about fentanyl and its risks, misinformation can persist in public discourse and among first responders on the front lines of the crisis. Daniel Meloy, a senior community engagement specialist at the drug recovery organizations Operation 2 Save Lives and QRT National, said he thinks of misinformation as “more of an unknown than it is an anxiety or a fear.”
“We’re experiencing it often before the information” can be understood and shared by public health and addiction medicine practitioners, Meloy said.
Some state and local governments are investing money from their share of the billions in opioid settlement funds in efforts to protect first responders from purported risks perpetuated through fentanyl misinformation.
In 2022 and 2023, 19 cities, towns, and counties across eight states used settlement funds to purchase drug detection devices for law enforcement agencies, spending just over $1 million altogether. Two mass spectrometers were purchased for at least $136,000 for the Greeley, Colorado, police department, “to protect those who are tasked with handling those substances.”
Del Pozo, the retired police chief, said fentanyl is present in most illicit opioids found at the scene of an arrest. But that “doesn’t mean you need to spend a lot of money on fentanyl detection for officer safety,” he said. If that spending decision is motivated by officer safety concerns, then it’s “misspent money,” del Pozo said.