Procedure and Follow-Up
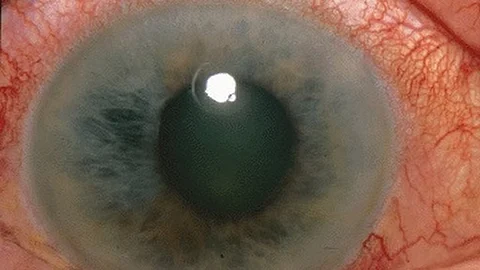
The transplantation process involved a specialized keratectomy to remove damaged tissue, followed by the placement of the iCEPS on the patients’ eyes, secured with therapeutic contact lenses. Postoperative care included antibiotics, corticosteroids, and regular monitoring to prevent complications. Safety was the primary concern, with adverse events closely monitored throughout the study. Metrics for efficacy included visual acuity, LSCD stage, and overall corneal health, which were evaluated at multiple intervals before and after surgery.
Of the four patients, the first two received iCEPS transplants mismatched for Human Leukocyte Antigen (HLA). After six months of follow-up, these initial transplants showed no signs of immunological rejection, leading to the decision to forgo additional immunosuppression in the subsequent two patients. Clinical improvements were noted in all participants, with stages of LSCD reduced in most cases. Patients 1 and 2 showed significant recovery from stage III to stage IA, while patient 3 improved from stage IIB to IA, with these improvements maintained throughout the follow-up. Patient 4 initially improved from stage III to IA but experienced a regression to stage IIB after one year, possibly due to subclinical immune responses.
Results and Safety Profile
The study reported no cases of tumor formation or immunological rejection. In total, 26 minor adverse events were observed across all patients during the 52-week observation, all of which were mild and manageable. An additional nine minor events were recorded during the extended safety monitoring, with no serious adverse effects. Improvement in visual acuity was most pronounced in patients 1 and 2, with stabilized or improved symptoms reported by all patients. Corneal opacification was reduced, and a decrease in corneal neovascularization was noted for patients 1 and 2, while the remaining patients showed stable or slightly increased neovascularization. Quality of life metrics improved for patients 1, 2, and 3, though patient 4 experienced some decline.
Conclusions and Future Directions
This pioneering first-in-human study demonstrated that iPSC-derived corneal epithelial cell sheets are well-tolerated, with no evidence of tumorigenicity or immune rejection. The results indicate a promising therapeutic option for LSCD patients, especially those who do not match HLA criteria for traditional transplants. While significant improvements were observed in LSCD staging and visual outcomes, further multicenter clinical trials are essential to confirm these findings on a broader scale.
These positive results underscore the potential of iPSC-derived therapies to overcome the limitations of current treatments for LSCD, providing a new avenue for patients who suffer from this debilitating condition.
Reference:
1. Kumar Malesu, Vijay. "Stem-cell implants restore vision in patients with corneal stem cell deficiency". News-Medical. https://www.news-medical.net/news/20241112/Stem-cell-implants-restore-vision-in-patients-with-corneal-stem-cell-deficiency.aspx. (accessed December 07, 2024).
(Input from various sources)
(Rehash/Ankur Deka/MSM)