A woman experienced a strange burning pain in her feet that gradually crept up her legs. Initially, she wrote it off as jet lag, having just returned from Thailand, Japan, and Hawaii. But when the pain grew more severe and her skin became hyper-sensitive, she went to see a doctor. [1,2]
The New England Journal of Medicine recently published a case report on the incident.
Early Doctor Visits Yield No Solutions
Her initial trip to the emergency room was unfruitful. Her exams were normal, so she was released. A few days later, the pain had moved to her torso and arms, along with a very bad headache. In desperation for answers, she went to another hospital, where physicians saw a greater-than-normal count of immune cells but no obvious reason for her illness. She was treated for her headache and released again.
Symptoms got worse, prompting hospitalization.
Things took a turn for the worse when she was confused, and her partner rushed her back to the hospital. Blood work and kidney function were normal, with no evidence of parasites in the blood. Yet, one peculiarity popped up — the level of eosinophils, a certain white blood cell involved in fighting infection, most notably parasites.
A stunning diagnosis: Eosinophilic meningitis
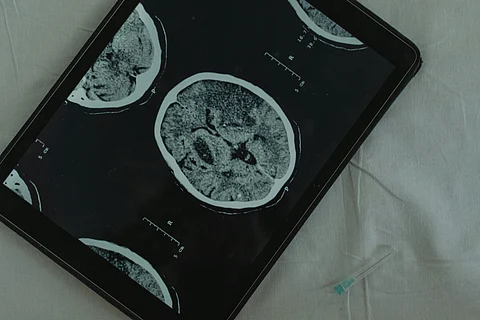
To get to the bottom of it, physicians conducted a lumbar puncture (spinal tap) to examine her cerebrospinal fluid. The test results indicated eosinophilic meningitis, an uncommon but serious brain and spinal cord infection typically caused by parasitic infestation.