The study also found another disturbing trend: organ offers were more likely to be accepted when the donor and patient were of the same race.
This pattern raises concerns about unconscious bias and systemic trust issues, possibly stemming from historical inequities in healthcare access and organ procurement. It also may suggest a preference for perceived immunological matching, though this is not always supported by clinical necessity.
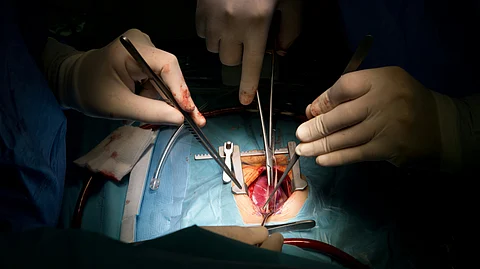
A typical example is that of a study published in JAMA on the differences in donor heart acceptance by race and gender of patients on the transplant waiting list in the U.S. [3]
In their study, it was noted that even within the same gender group, Black candidates had consistently lower acceptance rates for donor hearts than White candidates.