Heart in the throat!!
What does it represent?
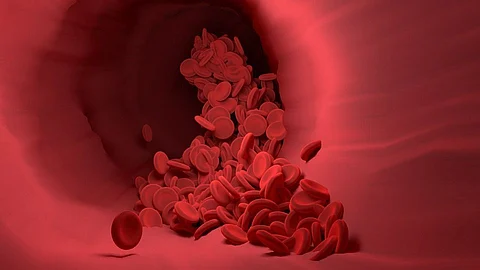
Patients with aortic regurgitation can see a palpable pulse of an aneurysm on the aortic arch. Aortic insufficiency results from the aortic valve's malfunctioning in aortic regurgitation, which causes the blood to flow back into the left ventricle. This causes the blood flow from the aorta to diminish, which causes the carotid artery to collapse. This condition is known as the CORRIGAN SIGN, and it is brilliantly illustrated in the video up top. It is among the crucial signs of aortic regurgitation.
The story of this sign begins with Sir Dominic Corrigan, the physicist who first noticed it. Thomas Watson later compared it to a water-hammer toy in 1844, 11 years after the discovery, and as a result, the name Corrigan sign was replaced with Watson pulse. Collapsing pulse, water hammer pulse, and pulsus celer are some of the alternate names.
What makes it hazardous?
As is well known, the left ventricles pump oxygenated blood throughout the body, and a reduction in blood flow to the aorta affects the delivery of blood to other organs. As blood flows back into the left ventricle, the left ventricle's pressure increases and the stroke volume reduces as a result. Low cardiac output can result in hypotension and, in extreme circumstances, cardiogenic shock.
What causes it?
Rheumatic disorders, where antibodies target our body cells, in this case, the valve, are the most frequent cause. Congenital abnormalities, the presence of only two leaflets (in this situation, the tricuspid valve's one leaflet is attached to the aortic valve), an aortic aneurysm, and degenerative illnesses are other common causes. The common risk factor is high blood pressure. Blood flow increases during this, which causes the valve to dilate and eventually become difficult to seal properly, resulting in regurgitation. Another cause could be connective tissue disorders and aortic inflammation.