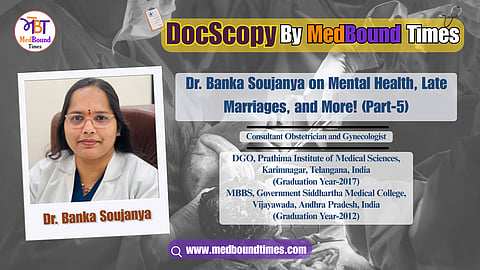
Dr. Banka Soujanya on Mental Health, Late Marriages, and Partner Involvement in Pregnancy (Part-5)
Dr. Banka Soujanya is a Consultant Obstetrician and Gynecologist. She completed her MBBS in 2012 from Government Siddhartha Medical College, Vijayawada, Andhra Pradesh, India. Later, she completed her post-graduation in DGO (Diploma in Gynecology and Obstetrics) in 2019 at Prathima Institute of Medical Sciences, Karimnagar, Telangana, India. She holds a Fellowship in Minimal Access Surgery (FMAS) and a Diploma in Minimal Access Surgery (DMAS). She also has a Diploma in ART (Germany, online).
She has a total of 9 years of experience. She is currently working at Reach Hospitals, Bachupally, and Dr. Vivaswan's Indira Clinic, Pragathinagar, Hyderabad, Telangana, India.
Dr. Banka Soujanya specifically deals with obstetrics and high-risk pregnancies, gynecological issues, laparoscopic surgeries, infertility issues, adolescent and menopausal issues, contraceptive advice, family planning, cervical cancer screening, and vaccination.
In this interview with MedBound Times, Dr. Banka Soujanya discusses mental and physical health, myths about overweight women can't go for normal delivery, the role of a partner during pregnancy, whether late marriages have an impact on C-section, and the need to measure depression post-delivery.
Himani Negi: When we are talking about certain myths, one question that often comes up is about a woman heavyweight. She is having a weight more than normal weight, so it is said that she will not be able to have a normal delivery and will require a C-section. So, what is your take on this? Because I think that during pregnancy, women gain weight. So, what is your perspective on this myth? Is it a part of a particular myth?
Dr. Banka Soujanya: A part of the concept is correct, as we gynecologists often ask obese women to control their weight gain during pregnancy. Because we can expect some complications in pregnancy, but not for the cesarean section, once a patient is obese, there is no clear-cut indication that she will end up in a cesarean section. In my practice women weighing around 120kgs have delivered vaginally without a need for C-section. So, weight is not an indicative factor for a cesarean section, but we advise women to monitor their weight gain during pregnancy.
We generally advise a weight gain of 5 to 6 Kg as there are chances of developing gestational hypertension or diabetes. If an obese woman develops gestational diabetes, it might lead to an excessive increase in fetal weight. If the baby weighs more than 4 Kg or 4.5 Kg, where the pelvis of the mother is not suitable for the baby to come out naturally, then we might go for a cesarean section.
In summary, obesity is indirectly related, but not directly or the sole reason. The complications associated with obesity might contribute to a cesarean section, but not just because of her weight.
Himani Negi: How common is the Edinburgh Scale test in India? If you have colleagues working in government hospitals, I would like to know if it is available for every patient. Is it something mandatory, or is it like some hospitals are providing this facility for postpartum depression? What do you think? Should it be mandatory?
Dr. Banka Soujanya: In the places where I have worked, such as the central government ESI Medical College or private practice, we usually don't use it regularly. When we conduct follow-up rounds in the post-operative days, if the patient appears abnormal or complains of symptoms, we assess her using the Edinburgh scale, which is not used for all patients worldwide.
I feel to make it should be made mandatory after the delivery of a baby and before discharging the patient, we provide the form to the patient, and whenever they're feeling low, they can return to see me. That process will help to assess whether the mother is happy or sad. I believe that we should use this now. It's important.
Himani Negi: I would like to know about pregnancy. We have a misconception from the grandparents' era that issues such as depression don't usually happen. They often believe that women have to work for nine months to have a healthy baby. Additionally, I would like to know if having a partner present during delivery is common. What do you think is the role of a partner during the pregnancy period? Mental health is as important as physical health, and whatever the mother is experiencing during the pregnancy matters as well. How common is it to have a partner during that labor, and how does their presence help?
Dr Banka Soujanya: The first thing is we shouldn't compare our generation or the current generation with our parents' generation. Nowadays, marriages are happening around 30 or 35. Some are facing infertility issues, so asking them to work continuously throughout the nine months of pregnancy might be challenging both physically and mentally.
Nowadays, we are seeing 24 or 25-year-old patients already diagnosed with conditions like diabetes. Therefore, comparisons with the previous generation or the parents should be avoided. In contrast, parents and in-laws may have high expectations that we shouldn't let these concerns interfere couple's happy journey of the nine months.
When I consult patients, I always tell my patients to call their husband also into my cabin throughout these nine months. She will be the one who will be bearing the baby physically. But her partner should provide emotional support to the wife. This often includes even the sharing of household activities, as many women are working nowadays, whether it might be homemakers or professional workers, whatever they are working. I'm happy to see my patients are working till eight or nine months, and then they are taking maternal leave.
So the husband's role is very crucial, not only physical, but emotional, sharing the household activities, coming for the consultation and checkups, staying with her in a scan room when the wife needs him, and also exercising. I insist that the woman go for a walk for 10 or 15 minutes along with her husband and talk for some time. This is the time that women get for themselves in these nine months of the journey.
We allow the partner to be in the delivery room. Sometimes the touch itself, such as holding hands, can offer a significant comfort to the mother during labour. In my case, too, I still remember when I was going through labor pain, my husband was by my side, and even when I was in pain, I squeezed his hand, like the pain burned my belly, but I gave the indirect pain to my husband also. He was there to guide me in such a way that words like now the contraction is happening, breathe in, breathe out, Just relax, take your time. Such are encouraging words, which are invaluable support.
Whether he's educated or not, being beside his wife is a great emotional support so that she can take the pain happily. So I usually allow at the time of delivery, also they'll be there, but some people are too sensitive. The husbands are so sensitive that they'll be scared to be in the labour room. In such cases, they can choose a supportive person in the labour room.
Generally, we don't allow patients requesting a C-section who claim that their daughter can't bear this pain, where such an option is strictly not allowed in the labour room. If you care enough and are courageous enough to support your wife, then you are welcome to be present in the labor room. If not, you will need to wait outside while I deliver the good news.
So if the husband is supportive and cares for his wife, having good bonding is needed to allow them. A strong bond starts not only in the delivery room, it starts early from the 5th month of pregnancy when they engage in doing their antenatal exercises, dietary management, walking, or the hospital visit and preparations for either a normal delivery or an emergency C-section, or a planned C-Section. Both of them should be involved throughout the entire nine-month journey.
Himani Negi: People are getting married at 30 or 35, which is very common. This raises a question: Is there a right time to conceive for a healthy normal delivery? Should one aim to conceive within a certain age to have a normal delivery, or is it acceptable to take their own time? What are your thoughts and considerations about the ideal age group for delivery?
Dr Banka Soujanya: If you have an option, it's best to plan before the age of 35. You can plan your family plan for one or two children to complete your family, and this could bring greater happiness, especially because of the rising infertility rates. Some people plan pregnancy after 35, 38, 40, or 42 because they want to settle financial and professional considerations, or plan to move abroad.
However, when you have an option, having a family is the most important thing for you. It is advisable to plan your pregnancies in less than 35 to 38 years at most, but not around the age of 40 or 42, because it could lead to complications, rising infertility rates, and a trend for normal delivery. As an obstetrician, we recognize that pregnancies at the age of 38 and above are precious and require care, so it has been considered with IVF.
If the mother is not cooperative and not progressing well, we don't take risks, and we prioritize safety. We avoid taking any unnecessary or excessive risk in the normal delivery process. If the baby shows signs of fetal distress, there might be some developmental delays later in life, might also be mentally or physically affected. So we have to give a healthy baby to the mother.
My main goal is that I want to deliver both mother and baby happily and healthily, whether it is a normal delivery or a C-section, both mother and baby should be healthy. There are a few scenarios, such as an excessive trial for normal deliveries, the baby goes into fetal distress, the heart rate drops to 60, or 70, and after 5 minutes baby is delivered leading to hypoxic damage to the brain that could land up into developmental delays, and even in learning disabilities. Therefore, if a mother is not a good candidate for normal delivery, we recommend a C-section to ensure a safe and healthy baby for the mother and the family.
Stay tuned for Part 6 discusses does conceiving late leads to a C-section, conditions where planned or emergency C-sections are done, and strategies to save both mother and baby.