Breaking the Silence on Oral Cancer: Dr. Bhuvan Nagpal on Awareness, Screening, and Stigma (Part-4)
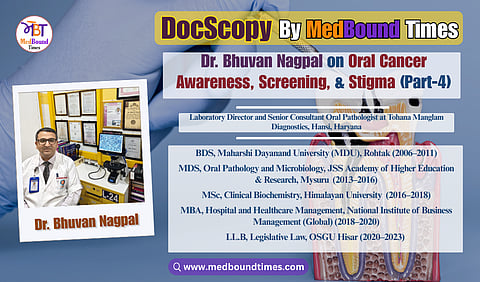
In an era where early diagnosis can mean the difference between timely intervention and advanced disease, oral pathology plays a quietly critical role in dentistry and cancer prevention. MedBound Times spoke with Dr. Bhuvan Nagpal, a distinguished oral and maxillofacial pathologist, clinical biochemist, and medico-legal consultant whose work spans diagnostics, research, public health, and healthcare law. With an extensive academic background that includes BDS (MDU, Rohtak), MDS (JSS, Mysuru), PGT in Head and Neck Oral Pathology, MSc, MBA, PGDMLS, LL.B, Ph.D (Honorary), and multiple professional certifications including CLQMS and FPFA (USA), Dr. Nagpal exemplifies lifelong learning and academic rigor, positioning himself at the intersection of precision diagnostics and multidisciplinary healthcare practice.
Currently serving as the Director of Tohana Manglam Diagnostics and a Business Partner at Manglam Diagnostics, Hansi, Haryana, Dr. Nagpal’s clinical focus lies in histopathological evaluation, early identification of oral potentially malignant disorders, and comprehensive head and neck diagnostics. Beyond clinical practice, he is the Founder and President of the Practicing Oral Pathologists and Microbiologists Association (POPMA) and the driving force behind the Centre for Oral Pathology and Maxillofacial Diagnostics (COPMD), India’s first dedicated chain of oral pathology diagnostic centres, aimed at strengthening the visibility and impact of oral pathology nationwide.
In this MedBound Times interview series, conducted by Dr. Akriti Mishra, Dr. Nagpal explores how community outreach, dental education, and digital platforms can enhance early screening and reduce stigma.
Dr. Akriti : How can community-level awareness campaigns or dental education help increase early screening uptake and reduce stigma around oral lesions?
Dr. Bhuvan Nagpal : Community-level awareness campaigns and dental education are indispensable tools for increasing early screening uptake and dismantling the stigma associated with oral lesions in India.
Let’s tackle each aspect:
Increasing Early Screening Uptake through Awareness Campaigns: When you go out into the community, be it rural villages or urban neighborhoods, and run awareness campaigns, you essentially bring knowledge and services to people’s doorsteps. For example, organizing free “Oral Cancer Screening Camps” in villages or at local health centers can encourage people to get checked. Many individuals might not seek out a dentist on their own, but if there’s a health camp with loudspeaker announcements saying “free mouth check-up for white patches or ulcers,” they may turn up out of curiosity or because it’s convenient. I’ve been involved in such camps, and once people come, we not only screen them but also use that opportunity to educate them about the early signs and risk factors. Regularly conducting these drives has been recommended as a strategy to catch cancers early.
Community awareness campaigns can take many forms like posters in local language showing pictures of what an early oral cancer looks like, street plays (nukkad natak) that dramatize the story of someone ignoring a lesion vs. someone catching it early, or short video screenings in village gatherings. The point is to make people aware that:
1) they should not ignore mouth lesions, and
2) getting screened is easy and beneficial. As awareness rises, people are more likely to present early.
We’ve seen this with other health issues, like how polio or HIV awareness drives improved testing behavior.
Also, leveraging local influencers or survivors in campaigns helps. For instance, having an oral cancer survivor from the community share their experience (like “I had a small ulcer, I got it checked, now I’m healthy thanks to early treatment”) can motivate others. Even involving community health workers (ASHA workers, etc.) to spread messages door-to-door can personalize the message.
Reducing Stigma around Oral Lesions: Stigma is a barrier because some people fear being ostracized or ashamed if they have a “cancer.” Awareness campaigns can humanize the issue. When we talk about oral cancer openly in the community, it starts to remove the taboo. People realize it’s a disease like any other, not a “curse” or something to hide. We emphasize that getting checked early is an act of strength, not something to be embarrassed about. For example, one major campaign that aired on TV featured a young oral cancer patient (Sunita) sharing her story openly, which made viewers empathize and also feel that they too can seek help without shame. Such narratives, when spread in communities, help reduce the fear and stigma.
Educational initiatives at the community level can also clarify misconceptions, like “oral cancer is not contagious” and that it can be cured if caught early, which alleviates some fear. I recall a survey indicating a majority of people, once aware, understood that cancer isn’t a divine punishment and can be treated. That shift in mindset is crucial so that people don’t avoid screenings out of fear of being labeled.
Role of Dental Education (Professional Training): Now on the dental education side which is about training the current and next generation of dentists to prioritize early detection. If every dentist graduating is taught that an oral cancer screening is a routine part of a dental exam (just like checking blood pressure might be a routine part of a physician’s exam), then screening rates will naturally go up. Dental schools can instill this by having students perform a number of oral cancer screenings in their clinical rotations. Also, including more about oral oncology in the curriculum can make young dentists more confident in identifying lesions and counseling patients.
Continuing education for practicing dentists is also valuable, like workshops on how to do a quick screening, how to do a biopsy, how to counsel a patient with a suspicious lesion. If dentists feel equipped and responsible, they will in turn educate their patients.
Dentists as Educators in the Community: Dentists can be champions of awareness themselves. A lot of dental clinics now participate in Oral Cancer Awareness Month (typically April) by offering free check-ups or giving talks in schools/colleges about the ill effects of tobacco. By doing so, they not only find cases early but also create an environment where talking about oral lesions is normal.
We should remember that in many parts of India, especially rural, the dentist might actually be the first healthcare person to notice a lesion (sometimes even before a primary doctor, as people might go to a dentist for a tooth problem and the dentist spots a lesion on the cheek). If that dentist is well-trained to handle it ethically and supportively, it can drastically change the outcome for that patient.
Community Involvement: Awareness campaigns that involve local community leaders (panchayat heads, teachers, religious leaders) can amplify the message. For instance, if a village leader announces “we have doctors coming to do mouth check-ups, please go, it’s a good thing,” people are more likely to participate. And if someone is found with a lesion, handling it sensitively and supportively in the community (ensuring they get help, not shaming them for a habit) will encourage others to come forward too.
Reducing Stigma Through Education: Education must also target the fact that having a risk habit is not something that deserves blame but rather support to quit. Sometimes people hide lesions because they feel guilty about their tobacco habit or worry they’ll be lectured. A compassionate approach in both community messaging and dental offices can reduce that barrier. For example, rather than scolding patients, we encourage them: “It’s good you came, now let’s take care of this.” Community talks by healthcare providers can emphasize that anyone can develop this disease and it’s nothing to be ashamed about. The key is to act early.
In conclusion, community-level campaigns and dental education go hand in hand: educate the public to demand and accept screenings, and educate dental professionals to provide and promote screenings. Together, this increases early detection. As more people get used to the idea of oral cancer screenings (just like women got used to mammograms or Pap smears over time due to campaigns), the uptake will improve. And as oral lesions and their risk factors are discussed more openly (in village meetings, schools, social media, everywhere), the mystery and stigma around them will diminish. People will realize an oral white patch is not a “dirty secret” but a medical condition that merits attention, just like a lump in the body would. That mindset change, fostered by education, is how we save lives through early diagnosis.
Dr. Akriti : What role can social media and digital outreach play in spreading awareness about oral cancer signs and encouraging regular dental check-ups?
Dr. Bhuvan Nagpal : Social media and digital outreach offer an unprecedented opportunity to spread awareness about oral cancer and encourage early, routine dental check-ups especially in a country like India with widespread smartphone use and diverse populations. These platforms can reach millions instantly, bridging gaps in traditional healthcare communication and access.
Here’s how they help specifically for oral cancer awareness and promoting dental check-ups:
Wider Reach and Targeting: India has a massive number of Internet and smartphone users, and platforms like Facebook, Instagram, Twitter, and WhatsApp are widely used. By leveraging these, we can reach demographics that traditional methods might miss, especially younger people. For example, a short informative video about the early signs of oral cancer (like a 1-minute clip showing what leukoplakia looks like and advising “if you see this, get checked”) can go viral or at least be shared widely, raising awareness. We can also target content to specific groups, say, a campaign on TikTok or Instagram Reels geared towards teenagers about not chewing gutkha, or informative posts in regional languages for specific communities.
Education with Visuals: Social media is a visual medium, and oral health is something you can show. We can share pictures of what a concerning lesion might look like (in a non-scary way, maybe a comparison of a normal cheek vs. one with a leukoplakia patch). Infographics listing the “5 warning signs of oral cancer” can be circulated. These simplify the information and make it easy to remember. I’ve seen posts that list, for instance, “painless mouth ulcer >2 weeks = see a dentist” that get a lot of engagement. The advantage is people can save these images, forward them to family (WhatsApp forwards can actually spread health info quickly), and refer back to them. It helps normalize the idea that mouths should be checked.
Interactive Engagement: Through live Q&A sessions, webinars, or Facebook Live events, dentists and oral pathologists can directly engage with the public. I’ve participated in live webinars during Oral Cancer Awareness Week where people from anywhere could ask questions, like “I have a red patch, what should I do?”, and we give real-time advice. This kind of interaction not only spreads information but also builds trust. It encourages people that it’s okay to talk about these issues and that experts are accessible.
Storytelling and Testimonials: Social media is great for storytelling. Sharing success stories or testimonials can encourage action. For instance, an oral cancer survivor’s story (with their permission) posted on YouTube or Facebook describing how they noticed something early, got treated, and are now doing well can be very motivating. It puts a human face to early detection. People might think, “If they benefited from a check-up, maybe I should get one too.” Similarly, a dentist could share a story of how they caught a lesion in a routine exam and potentially saved a life which underscores the value of regular check-ups.
Challenges and Campaigns: We’ve seen social media challenges for various causes (like the Ice Bucket Challenge for ALS). We could have something like a “Self Mouth Exam challenge” where people are encouraged to do a quick self-check and maybe post a thumbs-up (not showing their mouth, but just indicating they did it), to spread awareness of self-exams. Or a campaign hashtag like #CheckYourMouth that people and celebrities could amplify. In fact, involving celebrities on social media can greatly amplify the message. If a famous actor posts “I got my oral cancer screening this year, have you?” that could influence a lot of fans.
Reminders and Ease of Access: Digital outreach can also directly facilitate action. For example, apps or social media pages can send reminders: “It’s been 6 months since your last dental check-up, time to schedule one!” Many dental clinics now use WhatsApp to send such nudges to their patients. There are also oral health apps that guide users on how to do self-exams with their phone camera, or even allow users to take a photo of a lesion and get an AI evaluation or send it to a dentist (tele-dentistry). This kind of tele-screening is emerging: people in remote areas could, via an app, send a picture of a suspicious spot to a specialist who can advise if it looks concerning, all through digital means. That encourages people who are far from clinics to still seek some form of evaluation early.
Combating Misinformation: Social media does have the downside of sometimes spreading myths. But that means it’s also a place we need to be present to counter those myths. If someone, say, spreads a home remedy “just apply turmeric to any mouth ulcer and it will be fine,” we can respond with factual posts that say “if it doesn’t heal in 2 weeks, go to a dentist; turmeric or other home remedies are not proven to stop cancer.” By having a strong, factual presence online, we build a community that trusts professional advice.
Language and Localization: Digital content can be easily produced in multiple Indian languages and tailored to local contexts, which is huge for a country as diverse as India. We can have posters in Hindi, Punjabi, Tamil, etc., addressing local tobacco habits (like mishri use in certain areas, or paan in others) to make the message relatable. Social media allows these localized campaigns to flourish and find the right audience.
To give an example, during the COVID-19 lockdowns, a lot of dental professionals took to social media to continue patient engagement. They did oral hygiene challenges, diet tips for oral health, etc. We can harness that kind of momentum for oral cancer. A dentist on Instagram might do a weekly “Did you know?” series about oral cancer facts and encourage their followers to share it. Over time, this raises general awareness.
Finally, digital outreach breaks down access barriers. Not everyone reads newspapers or health magazines, but almost everyone has a mobile phone. Even in rural areas, many people use WhatsApp or watch YouTube. So social media can reach people who might not be reached by traditional health education. It can also direct them to resources, for instance, a post could include a link to find the nearest center offering free screening, or a phone number to call for help quitting tobacco, etc.
In summary, social media and digital outreach serve as powerful tools to educate, engage, and empower the public regarding oral cancer. By making information shareable and conversations public, they normalize the idea of checking one’s mouth and visiting the dentist regularly. Plus, the interactive nature can reduce fear as people may feel more motivated to act when they see others talking about it openly online. Of course, we have to be consistent and creative to keep the messages effective, but the potential impact on awareness is huge.
In this section, Dr. Bhuvan Nagpal underscores how strategic awareness initiatives and responsible use of digital platforms can normalize conversations around oral health, reduce stigma, and motivate individuals to seek timely dental evaluations. In Part 5, he turns the focus toward the future, discussing how emerging technologies, particularly AI-driven diagnostic tools, have the potential to enhance accuracy, expand access to screening, and significantly improve early oral cancer detection across India. Furthermore, he addresses the current research areas that need urgent focus for improving the oral cancer care in India.