Dr. Juhi Saxena (PT) on Gynae Physiotherapy Across Life Stages: Menstruation to Menopause (Part-5)
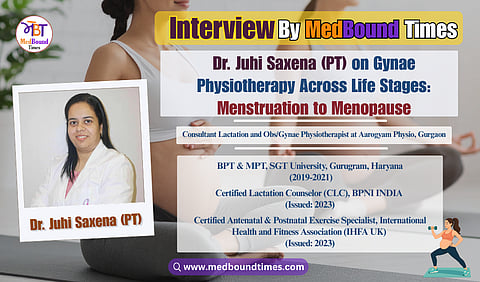
Many people still aren’t aware that OBG/Gynae physiotherapy exists—or how much it can improve women’s health at different stages of life. To spread awareness about this important and lesser-known aspect of physiotherapy, Dr. Pooja Bansal (PT) and Himani Negi from Medbound Times spoke with Dr. Juhi Saxena (PT), a women’s health physiotherapist.
Currently serving as a Consultant Lactation and Obs/Gynae Physiotherapist at Aarogyam Physio, Gurgaon, she has been actively working to raise awareness about this specialized field.
With a Bachelor’s degree in Physiotherapy from SGT University and a Master’s in Obs and Gynae Physiotherapy from the same institution, she highlights in this interview how physiotherapy plays a vital role in managing pregnancy-related discomfort, supporting postnatal recovery, addressing pelvic floor issues, and promoting overall wellness.
Dr. Pooja Bansal (PT): How exactly do physical therapists help in cases of pelvic floor issues, especially for the general public to understand? What do physical therapists actually do in these situations? Do they only prescribe exercises, or do they also provide emotional support and other forms of guidance?
Dr. Juhi Saxena (PT): When we treat a pelvic floor issue, it’s never just about exercises—it’s a holistic approach. We need to support the woman emotionally, mentally, and physically. It could be a mother or even a young woman—not every pelvic floor case is post-pregnancy related.
Understanding the woman’s psychology and also the mindset of the people around her is crucial. If she is mocked or made to feel ashamed at home, simply strengthening her muscles won’t help. That environment must be addressed. So, the first step is creating a safe space for her to open up. Once she feels comfortable, we assess her muscles, check for coordination with the brain, and then work on either strengthening or relaxation as required.
I remember one case where a young woman—not a mother—came with tight pelvic floor muscles. Each 40–45 minute session helped her relax, but by the next day, she would return in the same stressed state. For an entire week, despite working on her physically and mentally, there was no lasting improvement. Finally, I had a long conversation with her about her environment. That’s when I learned her mother-in-law had recently moved in, and constant remarks from her were triggering the woman’s pelvic floor to tighten again.
Once I addressed this and spoke calmly with her mother-in-law, the environment started to shift. Without changing a single thing in the treatment plan, we began to see results. Correcting her surroundings made all the difference. That’s why our role as physiotherapists goes beyond exercises—we also counsel patients, understand their psychology, and sometimes even involve their families. That emotional and environmental layer is often the most important part of healing.”
Dr. Pooja Bansal (PT): We often think of gynae physiotherapy as something mainly for pregnancy or post-delivery. But listening to you, the scope seems much wider—right from menstrual health and infertility to menopause. How would you explain the full role of a gynae physiotherapist across a woman’s life, and where do you think physiotherapists can step in to support patients alongside gynecologists?
Dr. Juhi Saxena (PT): We can actually begin very early. A physiotherapist working in gynecology and obstetrics doesn’t only step in during pregnancy or after delivery—the role starts much before that. For example, we can begin with something as simple yet important as teaching children about good and bad touch. Even boys and girls as young as 9 or 10 should be made aware.
From there, we can prepare young girls for menstruation before their first period, helping them understand what it really means. Menstruation is not just “bleeding”—it involves the whole body, from the uterus to the pelvic floor, and even affects day-to-day life. Gynecologists are already overburdened, and if physiotherapists step in to educate, guide, and break myths, it can be a huge support.
I’ve seen this personally—when I was younger, I had painful periods (dysmenorrhea). A gynecologist simply gave me hormone pills, which is the standard approach. But when I studied gynecological physiotherapy, I understood my pain better—it wasn’t only about the uterus contracting, but how my other muscles were reacting. With the right exercises and lifestyle changes, physiotherapy can actually help regulate menstrual cycles, manage PCOD-related weight gain, and reduce reliance on just medication.
Our role also extends into infertility care. Of course, we cannot solve every case, but we can support many couples. I’ve worked with women who had vaginismus—so severe that they didn’t let even a gynecologist examine them. But with therapy, they overcame it, conceived naturally, and went on to have healthy pregnancies and deliveries. That’s the power of physiotherapy.
Then comes postnatal care. From breastfeeding positions to posture correction, we guide mothers through recovery. Even years later, women in their 30s and 40s often come with urine leakage or prolapse issues, and physiotherapy can help them regain control.
And we must not forget menopause. This is rarely talked about, yet it brings physical, emotional, and sexual changes. Here too, physiotherapists can play a vital role in helping women adjust and manage symptoms.
So, the scope is actually endless. The challenge is awareness—people don’t always know when to reach out to us, and even the medical community often overlooks our role. But the truth is, physiotherapists can support women at every stage of life.
Himani Negi: Since we’re talking about the menstrual cycle and overall health, I was wondering—just like we go for regular health checkups every year, such as eye tests, blood tests, and so on—should physiotherapy also be part of these checkups? At what stage should one start consulting a physiotherapist? Even if someone has no visible problem, do you think they should still go, like a preventive full-body checkup?
Dr. Juhi Saxena (PT): These days, many private setups actually include physiotherapy in their health packages. Along with the physician and dietician, you’ll often get a complimentary consultation with a physiotherapist. A lot of private health institutes have started this. Even if your reports are normal, they still send you to a dietician for awareness about diet, a physician for a general check, and also a physiotherapist. When you meet us, we usually begin by asking how everything is going. If you open up about your concerns, a physiotherapist can definitely help.
But if you don’t share anything and just sit through the consultation, then later feel it was a waste of money, that mindset needs to change. It’s not only about the physiotherapist’s approach—it’s also about how you approach your own health. If you talk, if you bring up your issues, we can help. If you don’t, then you leave without getting value and may even badmouth the process. So, as individuals, we also need to shift our perspective toward preventive care.
Himani Negi: For blood tests, there are apps like HealthifyMe where I can book a home test without going to the hospital. But for physiotherapy, I feel like I need to meet the therapist in person—or maybe take an online consultation. Many office workers go for those health packages with 50, 70, or even 100 tests. So if I don’t feel I have any problem right now but still want to consult a physiotherapist, how should I start? Should I go for a kind of general checkup, where the therapist asks me some questions, or is it better to skip it if I don’t have complaints?
Dr. Juhi Saxena (PT): You can simply tell them, “I want a posture analysis.” From there, they can guide you. Even if you just say, “I feel a little tired” or “I’ve been sitting around a lot,” they’ll take it forward and help you. That’s a good way to begin, even without any clear issue.
Himani Negi: One more thing—how do we really decide if a professional suits us? In every field, there are good and bad experiences, and sometimes we’re not sure if things are moving in the right direction. Earning money is not wrong—after all, professionals have studied, worked hard, and deserve financial independence—but as patients, we still have our own concerns.
For example, one of my friends was told in her first month of pregnancy that a normal delivery wasn’t possible because she was overweight. She accepted it and didn’t take a second opinion, but later felt she should have. So, when we consult a physiotherapist—or any healthcare professional—what should we actually look at before deciding to continue with them? Can you share three to four key points patients should keep in mind?
Dr. Juhi Saxena (PT): The first thing you should always look at is qualification and authenticity. Don’t just go by Instagram or social media presence. Check if the person is actually a qualified healthcare professional, where they studied, and where they’ve practiced. You have every right to ask this, and a genuine professional will not be offended.
Second, see whether your goals align with theirs. For example, if your goal is to try for a normal delivery but your doctor immediately says it’s not possible without further discussion, then you may want to seek another opinion. If one professional denies it, you can consult others, but if three different professionals say the same thing, then it’s worth reconsidering.
Third, consider your personal connection with the professional. Even after one or five sessions, if you feel you cannot connect with them or you’re not on the same page, it’s okay to seek a second opinion.
Lastly, pay attention to feedback and surroundings. Sometimes reviews and opinions about a professional might be mixed—maybe others had a negative experience, but your personal experience is positive. In that case, trust your judgment, but remain cautious and aware.