What Really Works in Community Oral Health: Dr. Chintan Desai on Outreach, Trust, and Follow-Up (Part-5)
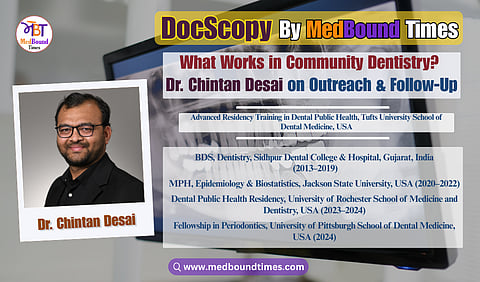
In this edition of MedBound Times, Himani Negi and Dr. Akriti Mishra speak with Dr. Chintan Desai, a Dental Public Health professional currently pursuing advanced residency training in Dental Public Health at the Tufts University School of Dental Medicine. With a strong foundation in clinical dentistry and a growing focus on population health, Dr. Desai represents a new generation of dentist–public health leaders working at the intersection of care delivery, research, and health equity.
A BDS graduate from Sidhpur Dental College, Gujarat, and holder of a Master of Public Health in Epidemiology and Biostatistics from Jackson State University, Dr. Desai has trained at renowned institutions including the University of Pittsburgh School of Dental Medicine and the Eastman Institute for Oral Health, University of Rochester. His work on NIH-funded projects and large public health initiatives has strengthened his expertise in data-driven research, program evaluation, and evidence-based dentistry.
Dr. Desai’s academic interests span oral–systemic health, periodontal disease, and epidemiological research using national health databases. He has co-authored peer-reviewed publications in journals such as Cureus and the Journal of Perinatology, presented at forums including AADOCR, NOHC, and the New York State Oral Health Summit, and serves as a peer reviewer for international dental and biomedical journals.
Beyond research, he is deeply committed to preventive care and health equity, contributing to school-based oral health programs, maternal and child initiatives, and community outreach addressing early childhood caries and access to care. His dedication to ethical, service-oriented dentistry has earned him selection as a Fellow of the International Pierre Fauchard Academy (India Section).
In the part 5 of this interview series at MedBound Times, conducted by Himani Negi and Dr. Akriti Mishra, Dr. Chintan Desai shares practical insights into effective community oral health outreach, highlighting the value of sustained engagement, trust building, and consistent follow up in underserved settings.
Dr. Akriti: Can you tell us about some specific outreach programs that you have been a part of in these years, and what worked well with the public, and what did not?
Dr. Chintan Desai: Yes, I have been fortunate to take part in several outreach programs in both India and the United States, and each experience taught me something important.
In India, I worked in a school based oral health program where we screened children, taught brushing techniques, and held tobacco awareness sessions. One of these programs took place on World No Tobacco Day on May 31st, where we spoke with students and parents about the dangers of tobacco. I also worked in a rural clinic where many families depended on visiting teams for dental guidance. These programs were successful because they focused on simple and practical education. Children responded well when we used visual demonstrations, and parents appreciated advice they could easily use at home. This showed me how effective outreach can be when it takes place in familiar community settings.
In the United States, my work expanded into public health research and organized community programs. At the Mississippi State Department of Health, I contributed to a ‘maternal oral health project‘ by working with data sets that support education for pregnant women. During my residency at the Eastman Institute for Oral Health in Rochester, I helped develop a dental home model for schoolchildren and took part in several health fairs. These programs worked well because they included follow up, partnerships with local organizations, and a clear path for families to receive care after the event.
What I have seen is that programs without continuity do not have the same impact. In many places in the United States, outreach sites are visited several times so that families know support is ongoing. In India, outreach teams often visit a location only once or return after many months. When there is a long gap, families may feel there is no continued support. These experiences taught me that sustainable community oral health programs depend on consistent engagement, strong partnerships, and long term presence.
Dr. Akriti: So, what strategies really work when you are reaching out to the underserved population? You talked about camps, school-based programs, and mobile clinics. So, based on your experience, what has worked the best?
Dr. Chintan Desai: Thank you for the question. From my experience, the mobile dental van has been the most effective strategy for reaching underserved communities. At regular health fairs, we only perform screenings and then refer patients to the main clinic. Many people do not follow up because they do not receive treatment on the spot and travel can be difficult for them.
The mobile van is more successful because it provides real care in the community. It can offer screenings, radiographs, cleanings, simple fillings, and extractions. It does not provide very specialized treatment, but it covers most basic needs. This makes people feel supported and removes many barriers. Another factor is consistency. The mobile van returns to the same location every few months, so families know that help will be available again. This steady presence builds trust and encourages people to seek care.
In my view, mobile vans and school programs work best because they bring treatment directly to the patient instead of only identifying problems and expecting them to travel for care. People respond when they can see something meaningful happening in front of them. If an outreach program only gives information through words, many patients may not feel the need to return. But when they see a demonstration or receive something useful, it creates a stronger connection.
In community outreach, we often provide small items such as a toothbrush, toothpaste, or floss. These are simple tools, but they help families start better habits at home. They also show that we care about their oral health beyond the short interaction at the event. When people know they will receive something helpful and also learn something practical, they are more likely to come back. This builds trust and makes the outreach more effective for the long term.
Dr. Akriti: In the community, which oral diseases (dental caries, periodontal diseases, or oral cancer) pose the greatest burden?
Dr. Chintan Desai: Thank you for the question. In both India and the United States, the conditions that create the greatest burden in community settings are dental caries and periodontal disease. These problems remain common because many families still struggle with limited access to routine care, preventive services, and early treatment. Children often come in with untreated cavities, and adults may not realize that periodontal disease is progressing until it becomes serious. These issues are closely linked to diet, hygiene habits, and overall health, which makes community education very important.
Oral cancer is another major concern, especially in India where tobacco chewing and smoking are common. During my work there, I saw many cases where patients came in at a late stage because they did not know the early signs or they delayed care. In the United States, the pattern is different, but some groups still face gaps in screening and early detection. These conditions show the need for strong preventive programs and better access to regular care.
Himani Negi: At present, India has certain drives and campaigns happening, but the required level of awareness is definitely missing. I believe many organizations in India are working toward the same goal. There are certain campaigns launched by the government as well, but again, the thing is, how many of these initiatives are actually translating into ground reality? That is the real question.
Dr. Chintan Desai: Yes, that is true. India has many campaigns and programs, but the challenge is making sure the message reaches people in a clear and consistent way. Awareness is improving, but there is still a gap between what is planned and what actually reaches the community. This is not because of a lack of effort, but because people may not always have access to information or may not know how to apply it in their daily lives.
In the United States, information is easier to access because most people have stable internet connections and use digital platforms every day. This allows us to share education through short videos, online messages, and virtual sessions. People can click a link and get reliable information instantly, which helps improve awareness.
Another important difference is how research programs and public health studies are organized. Many universities and clinics post simple recruitment flyers in public places with a barcode that people can scan. When they scan it, they learn about the study and decide if they want to join. Participants often receive small incentives, such as gift cards, which thank them for their time and encourage them to stay involved in the program. These incentives support participation and follow up, but they are not payments for quitting a habit. They simply recognize the effort people put into completing surveys or attending sessions.
During my previous residency, we worked on a tobacco related study. When someone enrolled, we gave them a small welcome kit with items like a toothbrush and toothpaste. This made them feel valued and supported from the beginning. Throughout the study, they received surveys every few months, and each completed survey came with a small gift card as a thank you. At the end, if they showed progress in reducing or stopping tobacco, they received a final card as well. The purpose was to encourage regular check ins and to help them stay motivated, not to pay them for quitting.
What I have learned is that steady engagement, clear messages, and small supportive incentives help people stay connected to the program. When they feel supported and when the information is easy to access, they are more willing to participate and make positive changes.
For example, when we plan a study that involves collecting new data, such as sending surveys to patients, we first check if our department has the funds to provide small incentives. If the budget is not enough, we apply for a grant to support the project. In the United States, incentives are an important part of research. They are not payments for personal information, but a way to thank participants for their time. Even a small gift card encourages people to join the study and complete the surveys. Without incentives, it is much harder to recruit participants and maintain good follow up. This method helps us gather reliable data and keeps people engaged throughout the study.
For the community outreach initiatives to grow beyond isolated efforts and achieve long-term change, they must be supported by evidence, ethical research practices, and enabling policies. Part 6 explores how outreach programs are planned, how data and surveys guide decisions, how research feeds into policy reform, and how emerging tools like artificial intelligence are reshaping community oral health delivery.